Database cloud migration in healthcare has become a response to real operational pressure rather than a strategic experiment. In hospitals, laboratory networks, and healthcare service providers, infrastructure ages faster than expected, data volumes continue to grow, and maintaining on-premises systems becomes harder and more expensive each year.
Databases sit at the center of this pressure. They store patient records, support clinical workflows, drive billing and reporting, and underpin regulatory compliance. Unlike applications or user interfaces, databases cannot be moved gradually without consequences. Any disruption at the data layer can affect patient care, financial accuracy, or audit readiness.
This is why cloud migration for healthcare database systems is treated as an engineering task where stability matters more than speed. Data, logic, performance, and security all need to remain intact while the execution environment changes.
In this article, we look at healthcare cloud migration from a database-first perspective. Based on real migration work, we explain why healthcare databases are difficult to move, what constraints shape migration decisions, and how automated conversion supports controlled healthcare data cloud migration database projects without redesigning core systems.
Why databases matter so much in Healthcare systems
In healthcare IT, databases are not passive storage layers. They actively shape how systems behave. Electronic Health Records, laboratory systems, imaging platforms, scheduling tools, billing engines, and insurance processing solutions all depend on databases that must remain predictable and available at all times.
Many healthcare systems were originally designed around the database layer. Over the years, critical logic moved into stored procedures, triggers, and functions. These elements control validations, workflow steps, financial rules, and reporting behavior that applications rely on.
As a result, healthcare databases usually contain:
- Large schemas with thousands of interconnected objects
- Procedural code refined over long periods of use
- Triggers enforcing clinical or billing rules
- Strong dependencies between tables, views, and procedures
From a migration standpoint, this means the database behaves like an application of its own. Treating it as a simple collection of tables is one of the most common and costly mistakes in cloud and healthcare database transformations.
Why on-premises databases are becoming a limitation
For years, on-premises infrastructure felt like the safest option for healthcare organizations. Direct control over hardware, networks, and access policies made compliance easier and risks more visible.
Over time, however, this model starts to create friction.
From the database side, the same issues appear repeatedly. Hardware refresh cycles are expensive and disruptive. Scaling databases for peak workloads is difficult to predict. Backup and disaster recovery setups grow more complex and fragile. Licensing models and vendor lock-in add long-term cost and reduce flexibility.
Taken together, these factors slow down healthcare cloud adoption database initiatives, even when the benefits of cloud platforms are clear.
What cloud migration actually means for Healthcare databases
In healthcare projects, cloud migration almost never means rebuilding systems from scratch. Most organizations have a firm requirement: the database must behave exactly the same way after migration as it did before.
Core clinical and administrative systems are validated, certified, and deeply embedded in daily operations. Changing schemas or rewriting logic would require long testing cycles and regulatory review, which is rarely acceptable.
In practice, cloud migration healthcare database work usually focuses on:
- Preserving existing schema structures
- Converting stored procedures, functions, and triggers
- Maintaining transactional behavior
- Ensuring queries return identical results
Migration success is measured by continuity. Applications should continue working as if nothing has changed.
Why heterogeneous environments complicate migration
Healthcare IT landscapes are rarely uniform. Systems are built over long periods, acquired through mergers, or delivered by different vendors. It is common to see several database technologies operating side by side.
Typical environments include Oracle, SQL Server, DB2 or Informix, and PostgreSQL. When migration begins, organizations often reassess these platforms as part of broader healthcare cloud migration services database initiatives.
Each database engine has its own SQL dialect, procedural language, data type handling, and transactional behavior. In healthcare systems, even small behavioral differences can lead to incorrect calculations or reporting issues. Heterogeneous migration is therefore less about syntax and more about preserving behavior.
Risks of cloud migration for Healthcare database systems
The risks of cloud migration for healthcare database platforms are closely tied to patient safety, financial integrity, and regulatory exposure.
Typical risk areas include loss of embedded logic, subtle changes in transaction handling, data inconsistencies during migration windows, and gaps in auditability. These risks increase significantly when migration relies on manual rewriting or loosely controlled processes.
Regulatory pressure adds another layer. Medical compliance cloud migration database requirements influence how data can be accessed, transferred, and validated throughout the process. Source databases often need to remain read-only, migration steps must be traceable, and data must stay within controlled environments.
Ignoring these constraints almost always leads to delays, rework, or failed projects.
Cloud migration for hospitals database platforms
Cloud migration for hospitals database systems brings additional operational pressure. Hospitals often run systems around the clock, leaving little room for downtime or experimentation.
In these environments, cloud migration hospitals database projects are usually staged and conservative. Parallel operation, rollback options, and detailed validation are standard requirements. The goal is to move databases without disrupting clinical workflows or administrative processes that depend on them.
Why automation becomes necessary
Manual database migration does not scale in healthcare environments. Large systems often contain tens of thousands of objects with complex dependencies. Rewriting them by hand is slow, expensive, and difficult to verify.
Manual approaches also create compliance challenges. It becomes harder to prove that migration steps were consistent and repeatable.
Automation helps by applying consistent rules across the entire database, reducing human error, shortening timelines, and producing outputs that can be reviewed and audited. This is especially important in healthcare IT cloud migration database projects, where traceability matters as much as correctness.
Automated database migration in Healthcare projects
In healthcare migrations, automation at the database level focuses on structure rather than application or procedural code. Healthcare databases often have large, complex schemas with many interdependent objects, and migrating these structures manually is both time-consuming and error-prone.
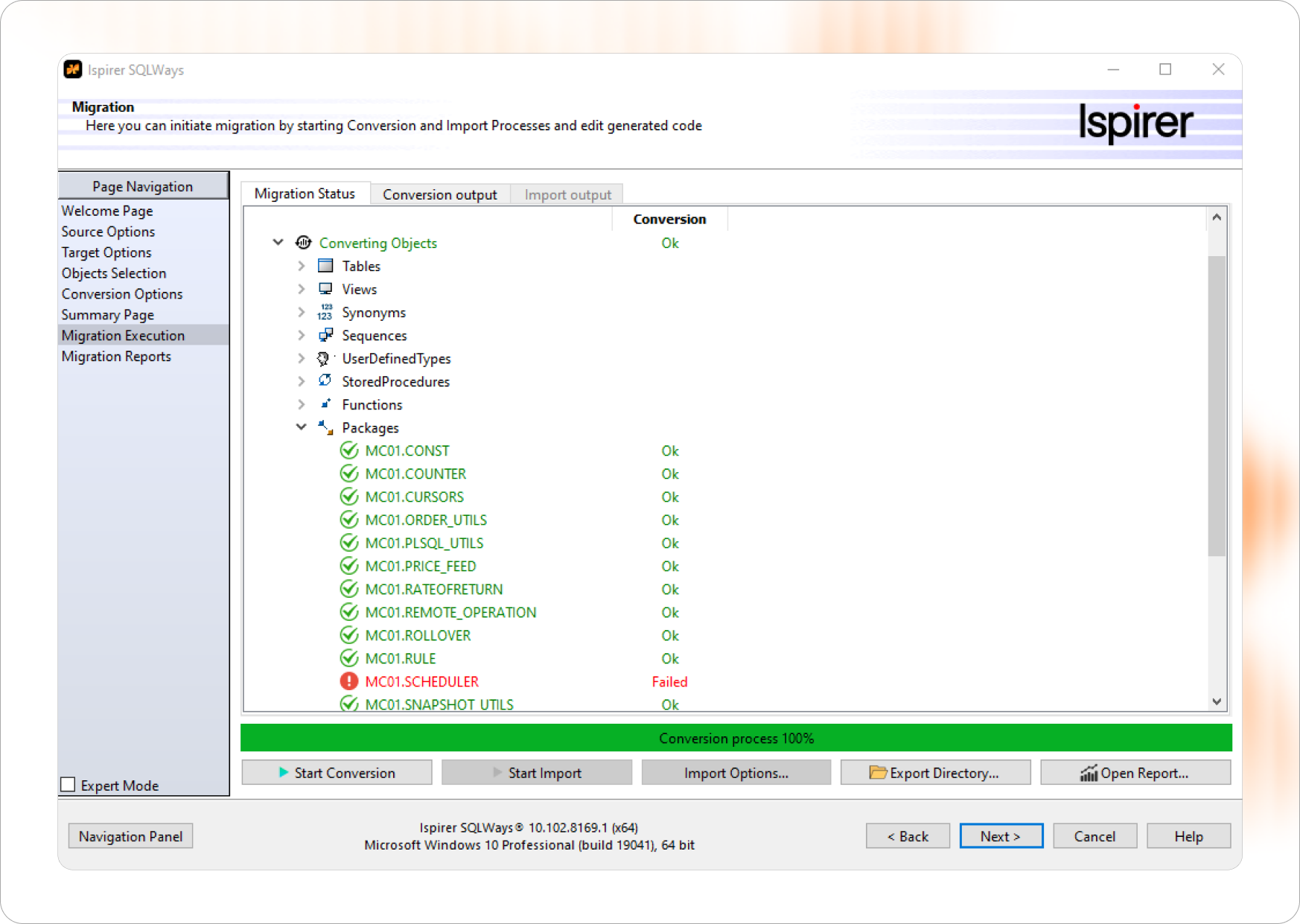
To address this challenge, we offer SQLWays, a database migration tool designed specifically for heterogeneous database schema conversion. SQLWays is part of the Ispirer Toolkit and is used to migrate database structures across different platforms while keeping the logical model intact.
What SQLWays migrates at the database level
SQLWays focuses on database schema objects and metadata. The tool supports migration of:
- Tables and columns
- Indexes and constraints
- Primary and foreign keys
- Sequences and schema-level dependencies
- Naming conventions and structural relationships
By migrating these elements together and taking dependencies into account, SQLWays helps preserve the structure and integrity of the database after migration.
How SQLWays handles heterogeneous database schemas
Different database platforms implement schema objects in different ways. SQLWays analyzes structural differences between source and target databases, including data types, constraints, reserved words, and identifier rules.
When direct equivalents are not available, the tool applies transformation rules and records these decisions in conversion reports. This makes schema conversion predictable and avoids silent structural changes that could affect application behavior later.
Working within Healthcare security and compliance constraints
SQLWays is designed to operate within strict security boundaries typical for healthcare environments. It does not modify the source database and works with controlled access to database metadata.
The tool can be deployed on Windows, Linux, or Unix systems and supports on-premises, cloud, and hybrid database environments. This allows healthcare organizations to migrate database schemas gradually while keeping production systems stable.
Transparency and validation support
SQLWays generates detailed reports describing schema conversion results. These reports help teams review converted objects, verify structural consistency, and document migration decisions.
By focusing strictly on database schema migration, controlled automation, and transparent reporting, SQLWays supports healthcare projects where database structures must be migrated accurately without redesign and without touching application or procedural code.
Cloud migration strategy for Healthcare database environments
A cloud migration strategy for healthcare database systems is not a roadmap toward modernization. In most cases, it is a framework for controlling risk. The goal is to move databases to a new environment while keeping clinical, administrative, and financial systems stable and predictable.
In healthcare projects, strategy is less about choosing a cloud provider and more about defining how change is introduced, validated, and limited. A successful strategy aligns technical decisions with regulatory constraints, operational realities, and the actual structure of healthcare databases.
Treat the database as a complete system
Healthcare databases should be approached as integrated systems rather than collections of independent objects. Schemas, procedural logic, dependencies, and performance characteristics are tightly connected. Decisions made at the level of individual tables or procedures often lead to hidden regressions later in the project.
Preserve behavior before introducing change
One of the most common strategic mistakes is trying to improve or optimize the database during migration. In healthcare environments, this almost always increases risk and extends timelines.
A sound strategy focuses first on behavioral equivalence. The database in the cloud should return the same results, follow the same transactional rules, and support the same workflows as before.
Limit manual intervention and control it carefully
Automation provides a consistent baseline for conversion. Manual changes should be limited to clearly identified edge cases, documented, and easy to trace.
Build validation into every stage
Schema comparisons, logic testing, and scenario validation should be part of the migration process from the beginning, not postponed until the end.
Design the strategy around regulatory constraints
Regulatory requirements shape the migration strategy itself. Migration steps must be transparent, repeatable, and easy to explain from a compliance perspective.
Assume hybrid operation as the default state
Most healthcare organizations migrate gradually. Strategies should support parallel operation, staged rollout, and safe rollback without disrupting ongoing processes.

Final thoughts
Database-focused healthcare cloud migration database projects are not routine infrastructure updates. They affect systems directly involved in patient care and daily operations.
Successful migration depends on preserving schema, logic, performance, and security while changing where the database runs. Experience shows that careful planning and automation make this possible without unnecessary risk.
As cloud adoption continues across healthcare, disciplined database migration will remain a foundation for stable, compliant, and scalable systems.



